Paediatric Cardiology
Paediatric Cardiology
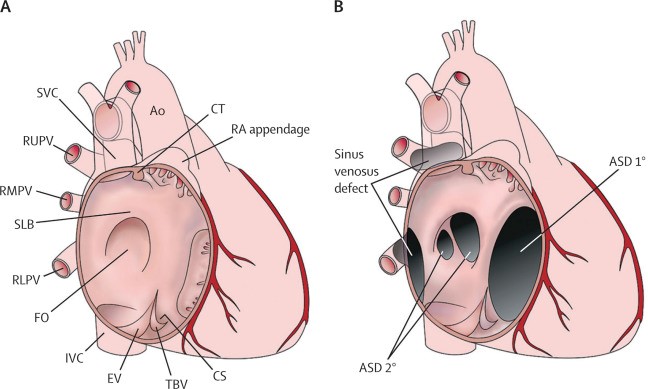
Atrial Septal Defect
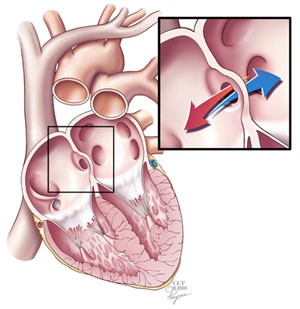
What happens during the closure procedure?
The procedure is performed while your child is under a general anaesthetic. This means that your child will be asleep during the procedure. Not every ASD can be closed with heart catheterization. Therefore, we first need to measure the ASD to make sure it can be closed with a device in the catheterization lab.
When your child is asleep, we will do a test called a transesophageal echocardiogram. “Echocardiogram” ,”Transesophageal” means we do the ultrasound with a small probe that is placed in your child’s esophagus, the tube that connects the mouth to the stomach. This test will measure the size of the hole and help place the closure device.
- If the test shows that the hole is too big to close with the device, we will wake up your child and send him or her to the recovery room. Your child’s cardiologist will discuss the next steps with you and your child.
- If the hole is small enough and in the right position, we will go on with the catheterization.
Coarctation of the aorta repair
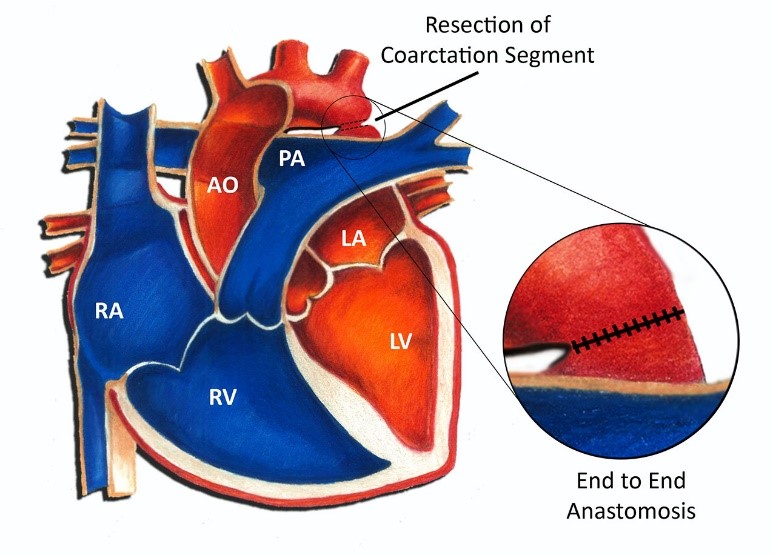
The ductus arteriosus is a blood vessel that is normally present in a fetus and has special tissue in its wall that causes it to close in the first hours or days of life. Coarctation may be caused by the presence of extra ductal tissue extending into the adjacent aorta which results in aortic narrowing as the ductal tissue contracts.
In babies with coarctation, the aortic arch may also be small (hypoplastic). Coarctation may also occur with other cardiac defects, typically involving the left side of the heart. The defects most commonly seen with coarctation are bicuspid aortic valve and ventricular septal defect. Coarctation may also be seen as a part of more complex single ventricle heart defects. Coarctation of the aorta is common in some patients with chromosomal abnormalities, such as Turner’s syndrome.
In the presence of a coarctation, the left ventricle has to work harder, since it must generate a higher pressure than normal to force blood through the narrow segment of aorta to the lower part of the body. If the narrowing is very severe, the ventricle may not be strong enough to perform this extra work, resulting in congestive heart failure or inadequate blood flow to the organs of the body.
Patent Ductus Arteriosus (PDA) & Repair/ Closure
At birth, the placenta is removed when the umbilical cord is cut. Your baby’s lungs must now provide oxygen to his or her body. As your baby takes the first breath, the blood vessels in the lungs open up, and blood begins to flow through them to pick up oxygen. At this point, the ductus arteriosus is not needed to bypass the lungs. Under normal circumstances, within the first few days after birth, the ductus arteriosus closes and blood no longer passes through it.
In some babies, however, the ductus arteriosus remains open (patent) and the condition now becomes known as patent ductus arteriosus (PDA). The opening between the aorta and the pulmonary artery allows oxygen-rich (red) blood to recirculate into the lungs. Patent ductus arteriosus occurs twice as often in girls as in boys.
PDA Repair or Closure
The majority of children and some infants with PDA are candidates for repair in the cardiac cath lab. The goal is to repair the PDA before the lungs become diseased from too much blood flow and pressure and to restore an efficient pattern of blood flow. Surgical repair is also indicated if one of the previously mentioned conservative treatments have not been successful.
Repair is usually indicated in infants younger than 6 months of age who have large defects that are causing symptoms, such as poor weight gain and rapid breathing. For infants who do not exhibit symptoms, the repair may often be delayed until after 6 to 12 months of age. Your child’s cardiologist will recommend when the repair should be performed. Transcatheter coil closure of the PDA is frequently performed first if possible because it is minimally invasive. Children need to be at least 5 kg to be considered for transcatheter closure. Thus, premature infants, because of their small size, are not candidates for this procedure, and require surgical closure of the PDA. Your child’s PDA may be repaired surgically in the operating room.
The surgical repair, also called PDA ligation, is performed under general anaesthesia. The procedure involves closing the open PDA with stitches or clips in order to prevent the surplus blood from entering your child’s lungs.
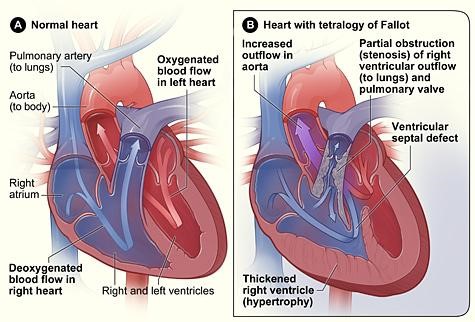
Tetralogy of Fallot (TOF)
Ventricular Septal Defect (VSD) & Closure/ Repair
What happens during the closure procedure?
- If the test shows that the hole is too big to close with the device, we will wake up your child and send him or her to the recovery room. Your child’s cardiologist will discuss the next steps with you and your child.
- If the hole is small enough and in the right position, we will go on with the catheterization.

Aarav Medicare team is ready to look after all your medical emergency needs. We will Take care of your health.
Saurav
Why Aarav Medicare?

Highly Qualified Specialists
Best Specialist Doctors for all the Treatment and Procedures. Get Free Online Consutations.

State Of The Art Facility
Finest Hospitals with all the modern Medical Equipment and Best Patient Care.

