Obstetrics and Gynaecology
Obstetrics and Gynaecology
Cervical Cerclage
Cervical cerclage, also known as a cervical stitch, is a treatment for cervical incompetence or insufficiency, when the cervix starts to shorten and open too early during a pregnancy causing either a late miscarriage or preterm birth. Usually the treatment is done in the second trimester of pregnancy, for a woman who had either one or more late miscarriages in the past.
The treatment consists of a strong suture being inserted into and around the cervix early in the pregnancy, usually between weeks 12 to 14, and then removed towards the end of the pregnancy when the greatest risk of miscarriage has passed.
In women with a prior spontaneous preterm birth and who are pregnant with one baby, and have shortening of the cervical length less than 25 mm, a cerclage prevents a preterm birth and reduces death and illness in the baby.There is no evidence that cerclage is effective in a multiple gestation pregnancy for preventing preterm births and reducing perinatal deaths or neonatal morbidity.
Colporrhaphy
Anterior repair
Anterior repair is used to tighten the front (anterior) wall of the vagina. It is used when the bladder drops out of its normal position and bulges into the front of the vagina, causing the front wall of the vagina to sag. This condition is known as anterior wall prolapse, cystocele or dropped bladder. During the surgery, the bladder is pushed back into its normal position and the support tissue between the front of the vagina and the bladder is tightened and reinforced. The procedure is also called an anterior vaginal wall repair or anterior colporrhaphy.Posterior repair
Posterior repair is used to tighten the back (posterior) wall of the vagina. It is used when the rectum drops out of its normal position and bulges into the back of the vagina, causing the back wall of the vagina to sag, which may result in bowel dysfunction. This condition is known as posterior wall prolapse, rectocele or fallen rectum. During the surgery the rectum is pushed back into to its normal position, and the support tissue between the back of the vagina and the rectum is tightened and reinforced. The procedure is also called a posterior vaginal wall repair or posterior colporrhaphy.Salpingo-oophorectomy
Salpingo-oophorectomy is surgery to remove the ovaries and fallopian tubes.Removal of one ovary and fallopian tube is called a unilateral salpingo-oophorectomy. When both are removed, it’s called a bilateral salpingo-oophorectomy. This procedure is used to treat a variety of conditions, including ovarian cancer. Sometimes healthy ovaries and fallopian tubes are removed to help prevent ovarian cancer in women who are at particularly high risk. This is known as a risk-reducing salpingo-oophorectomy. This surgery has been shown to be highly effective in lowering the risk of breast and ovarian cancer. Learn more about the causes and risk factors for ovarian cancer. Salpingo-oophorectomy doesn’t involve removal of the uterus (hysterectomy). But it’s not uncommon for both procedures to be performed at the same time.Who should have this procedure?
You might be a good candidate for this procedure if you need treatment for:- Ovarian cancer
- Endometriosis
- Benign tumours, cysts, or abscesses
- Ovarian torsion (twisting of the ovary)
- Pelvic infection
- Ectopic pregnancy
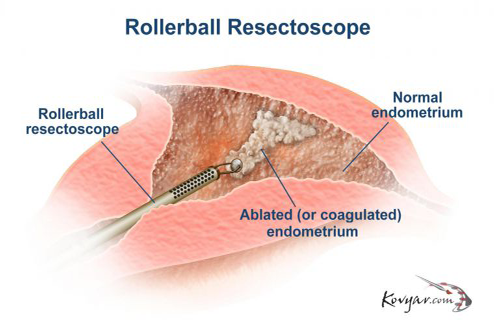
Endometrial Ablation
An endometrial ablation is a procedure your doctor might consider if you bleed between your menstrual periods, have a heavy flow, or have periods that last a long time. If medicine doesn’t help, your doctor might suggest endometrial ablation. It can curb the bleeding or stop it totally.
Heavy menstrual bleeding can have many causes. Changing hormones might be the reason. Or it could be fibroids and polyps growing in your uterus.
Endometrial ablation removes the endometrium, which is the lining of the uterus. In most cases, this stops you from having periods. If it doesn’t completely stop your periods, your flow should at least return to normal or be very light.
Hymenotomy
Hymenotomy is a medical procedure involving the surgical removal or opening of the hymen. It is often performed on patients with an imperforate or septate hymen, or other situations where the hymen is unusually thick or rigid such as Microperforte Hymen. In the case of a person with a hymen without any opening, an opening may be created in order to facilitate menstruation. In situations where the opening is extremely small or the band(s) of a septate hymen limit access to the vaginal opening, the individual may elect for hymenotomy to allow for comfortable sexual penetration of their vagina, or to relieve pain or discomfort that occurs when inserting/removing tampons. Sexual intercourse would not normally be adversely affected by a hymenotomy.
Cosmetic Surgery: Focused on Enhancing Appearance
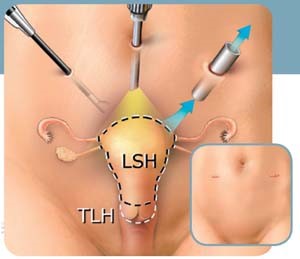
Unlike hysterectomy wherein the surgeon can make the incision either in the abdomen or the vagina to access the uterus, hysterotomy is performed exclusively via the abdomen. The incision is generally smaller when compared to the one used in hysterectomy. Both procedures can be performed under general anaesthesia.
Hysterotomy is the widely preferred technique for open foetal surgery. It is also the operation of choice if the uterus needs to be operated on during pregnancy or if a woman decides to abort the foetus after the first trimester. If the procedure is to be performed for delayed abortion, it is done the same way as caesarean section.
Myomectomy
Myomectomy is the surgical removal of fibroids from the uterus. It allows the uterus to be left in place and, for some women, makes pregnancy more likely than before. Myomectomy is the preferred fibroid treatment for women who want to become pregnant. After myomectomy, your chances of pregnancy may be improved but are not guaranteed.
Before myomectomy, shrinking fibroids with gonadotropin-releasing hormone analogue (GnRH-a) therapy may reduce blood loss from the surgery. GnRH-a therapy lowers the amount of estrogen your body makes. If you have bleeding from a fibroid, GnRH-a therapy can also improve anemia before surgery by stopping uterine bleeding for several months.
Surgical methods for myomectomy include:
- Hysteroscopy, which involves inserting a lighted viewing instrument through the vagina and into the uterus.
- Laparoscopy, which uses a lighted viewing instrument and one or more small cuts (incisions) in the abdomen.
- Laparotomy, which uses a larger incision in the abdomen.
The method depends upon:
Size, location, and number of fibroids.
Hysteroscopy can be used to remove fibroids on the inner wall of the uterus that have not grown deep into the uterine wall. - Laparoscopy is usually reserved for removing one or two fibroids, up to about 2 in. (5.1 cm) across, that are growing on the outside of the uterus.
- Laparotomy is used to remove large fibroids, many fibroids, or fibroids that have grown deep into the uterine wall.
- Need to correct urinary or bowel problems. To repair these problems without causing organ damage, laparotomy is usually needed.
Tubal Reversal
Vaginectomy
Vulvectomy
Vulvectomy refers to a gynaecological procedure in which the vulva is partly or completely removed. The procedure is usually performed as a last resort in certain cases of cancer, vulvar dysplasia, vulvar intraepithelial neoplasia, or female genital mutilation. Although there may be severe pain in the groin area after the procedure, for a number of weeks, sexual function is generally still possible but limited.
Simple vulvectomy
simple vulvectomy can be either complete (more than 80% of the vulvar area) or partial (less than 80% of vulvar area). It removes the skin and superficial subcutaneous tissues. a radical vulvectomy is the same with regard to complete or partial, however, includes removal of skin and deep subcutaneous tissue. An inguinofemoral lymphadenectomy may be performed along with a radical vulvectomy (whether partial or complete) on one or both sides if spread of a cancer is suspected.
Simple partial vulvectomy
Simple partial vulvectomy is the least severe, only removing the affected portion of the vulva.’Skinning vulvectomy’ involves the removal of the top layer of vulvar skin (the external female genital organs, including the clitoris, vaginal lips and the opening of the vagina). In this case skin grafts from other parts of the body may be needed to cover the area. There are two types of Skinning Vulvectomy, the ‘partial skinning vulvectomy’ and the ‘total skinning vulvectomy’. The objective of the first one is the preservation of the cosmetic and functional integrity of the vulva in younger and sexually active patients, in whom a steady increase in the incidence of vulvar intraepithelial neoplasia has been observed in the last decade. Meanwhile, the objective of the total skinning vulvectomy is to remove the entire vulva with total skin graft replacement in patients with an entire vulvar cancer involvement. ‘Modified radical vulvectomy’ involves the removal of vulva containing cancer and some of the normal tissue around it.

Aarav Medicare team is ready to look after all your medical emergency needs. We will Take care of your health.
Saurav
Why Aarav Medicare?

Highly Qualified Specialists
Best Specialist Doctors for all the Treatment and Procedures. Get Free Online Consutations.

State Of The Art Facility
Finest Hospitals with all the modern Medical Equipment and Best Patient Care.

