Cardiology/CTVS
Cardiology/CTVS
Adult Congenital Heart Surgery
Adults with congenital heart disease (CHD) generally fall into two categories: patients who have been recognized, treated, and followed during their pediatric years and subsequently require follow-up during their adult years; and the de novo, previously unrecognized adults who may or may not be symptomatic at the time of diagnosis. Despite the complexity of this patient population and a well-defined need for subspecialty care, the average adult with CHD is followed primarily by a generalist. It is essential, therefore, that all physicians be familiar with the unique clinical presentations of these patients and have a general understanding of their anatomy and its consequences to facilitate the proper timing of referral for percutaneous, electrophysiologic, and surgical interventions. The clinical course of CHD in the adult is most dependent on the anatomic lesions present and the timing and manner of repair. These lesions can be divided into three general categories
- Simple shunt Lesions
- Obstructive Lesions
- Complex Lesions (acyanotic and cyanotic)
Angioplasty(PTCA)
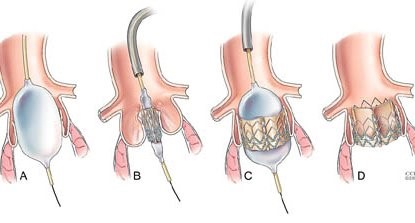
Percutaneous transluminal coronary angioplasty (PTCA) is a procedure to open narrowed or blocked blood vessels that supply blood to the heart. These blood vessels are called the coronary arteries. A coronary artery stent is a small, metal mesh tube that expands inside a coronary artery
PTCA is a minimally invasive procedure to open up blocked coronary arteries, allowing blood to circulate unobstructed to the heart muscle.

The procedure begins with the doctor injecting some local anesthesia into the groin area and putting a needle into the femoral artery, the blood vessel that runs down the leg. A guide wire is placed through the needle and the needle is removed. An introducer is then placed over the guide wire, after which the wire is removed. A different sized guide wire is put in its place.
Next, a long narrow tube called a diagnostic catheter is advanced through the introducer over the guide wire, into the blood vessel. This catheter is then guided to the aorta and the guide wire is removed. Once the catheter is placed in the opening or ostium of one the coronary arteries, the doctor injects dye and takes an x-ray.
If a treatable blockage is noted, the first catheter is exchanged for a guiding catheter. Once the guiding catheter is in place, a guide wire is advanced across the blockage, then a balloon catheter is advanced to the blockage site. The balloon is inflated for a few seconds to compress the blockage against the artery wall. Then the balloon is deflated.
The doctor may repeat this a few times, each time pumping up the balloon a little more to widen the passage for the blood to flow through. This treatment may be repeated at each blocked site in the coronary arteries. A device called a stent may be placed within the coronary artery to keep the vessel open. Once the compression has been performed, contrast media is injected and an x-ray is taken to check for any change in the arteries. Following this, the catheter is removed and the procedure is completed.
Aortic Stenosis


Aortic stenosis is a condition that results from narrowing of the aortic valve of the heart. This valve normally allows blood flow to be pumped from the main chamber of your heart to the rest of your body. When this valve becomes significantly narrowed, it can put an increased amount of stress and pressure on the heart muscle. This can lead to symptoms of chest discomfort, shortness of breath, leg swelling, fatigue, lightheadedness, syncope (passing out spells), and even sudden death.
TAVI or TAVR stands for transcatheter aortic valve replacement. Currently, this is an option for patients with severe aortic stenosis causing symptoms that are too high risk for standard valve replacement surgery. During a TAVI or TAVR procedure, a catheter about the size of a pen, is inserted in the artery in the leg and carefully passed up into the heart. One type of TAVR valve, made of bovine (cow) tissue and supported on a metal stent, is then implanted inside the narrowed valve resulting in a normal functioning aortic valve. With a TAVR procedure, the patient does not need the chest opened for surgery or put on a heart-lung (bypass) machine.
Is TAVI/TAVR safe?
The TAVI/TAVR procedure has been done in over 50,000 patients worldwide. It was FDA approved in November 2011. In the research trials evaluating TAVI/TAVR, it was shown to significantly allow patients to live longer and with better quality of life when compared to treating with medicines only. As with any heart procedure, TAVI/TAVR has its own risks. These risks can be discussed with your physician at the time of your appointment.
Where is TAVI/TAVR being done? Who does this procedure?
Currently, the FDA is allowing TAVI/TAVR to be done at hospitals with a high level of cardiac and heart surgery experience. The procedure is performed by a team of physicians including both cardiologists and heart surgeons. At this time, Dr. Ravi Ramana of Heart Care Centers, is performing this procedure at Advocate Christ Medical Center.
Atrial Septal Defect (ASD) & Closure/ Repair
The atrial septal defect (ASD) is the most common congenital heart defect encountered in adults, accounting for up to 15% of all adult CHD, It results from the failure of proper embryologic development of the atrial septum. There are many different types of ASD , the most common of which is the secundum ASD, in which the defect occurs in the middle of the atrial septum.
The flow of blood across the defect (shunt) is determined by the size of the defect and the compliance of the atria. ASD should be suspected whenever right heart enlargement is present without an alternative explanation. Occasionally, patients present late in life with ASD-related symptoms when the left atrial pressure increases because of a stiff left ventricle and diastolic dysfunction, usually the result of long-standing hypertension or coronary artery disease, resulting in increased shunt.
The larger the left-to-right shunt is in patients with ASD, the greater is the risk for long-term complications, such as atrial fibrillation and pulmonary hypertension. The latter condition affects up to 15% of adults with ASD and, if it remains uncorrected, it can result in Eisenmenger’s syndrome (see later). Another condition associated with ASD is stroke, which presumably results from paradoxical embolization—blood clots forming in the extremities and reaching the cerebral circulation by passing through the ASD.
Other, less-common variations of ASD include the sinus venosus ASD, in which there is abnormal fusion of the vena cava (superior or inferior) to the left atrium. This defect is almost always associated with partial anomalous return of the pulmonary veins (right superior or both right pulmonary veins drain into the right atrium). The primum ASD involves the lower portion of the atrial septum and typically affects the ventricular septum as well (the atrioventricular [AV] canal defect). Both AV valves are structurally abnormal, and the mitral valve is typically cleft. The least common form of ASD involves unroofing of the coronary sinus, which results in shunting into the left atrium. At this time, only the secundum ASD has been successfully occluded through percutaneous means.
What happens during the closure procedure?
When your child is asleep, we will do a test called a transesophageal echocardiogram. “Echocardiogram” ,”Transesophageal” means we do the ultrasound with a small probe that is placed in your child’s esophagus, the tube that connects the mouth to the stomach. This test will measure the size of the hole and help place the closure device.
- If the test shows that the hole is too big to close with the device, we will wake up your child and send him or her to the recovery room. Your child’s cardiologist will discuss the next steps with you and your child.
- If the hole is small enough and in the right position, we will go on with the catheterization.
During the catheterization, the doctor puts a catheter with a small deflated balloon on the tip through the blood vessel to the hole. The balloon is inflated to measure the size of the hole again. If the hole can be closed with the device, the doctor puts the closure device inside the catheter and places the device into the hole. Once the device is in place, the doctor takes out the catheter and covers the cut on your child’s leg with a bandage.
Coarctation of the Aorta
Coronary Artery Bypass Graft (CABG)

Coronary artery bypass grafting (CABG) is a surgical procedure that aims to improve blood flow to the heart. CABG is advised for people with severe coronary heart disease, a condition in which plaque builds up inside coronary arteries. The coronary arteries supply oxygen and nutrients to the heart muscle.
Coronary artery bypass grafting (CABG) is a type of surgery that improves blood flow to the heart. Surgeons use CABG to treat people who have severe coronary heart disease (CHD).
CHD is a disease in which a waxy substance called plaque (plak) builds up inside the coronary arteries. These arteries supply oxygen-rich blood to your heart.
Over time, plaque can harden or rupture (break open). Hardened plaque narrows the coronary arteries and reduces the flow of oxygen-rich blood to the heart. This can cause chest pain or discomfort called angina (an-JI-nuh or AN-juh-nuh).
If the plaque ruptures, a blood clot can form on its surface. A large blood clot can mostly or completely block blood flow through a coronary artery. This is the most common cause of a heart attack. Over time, ruptured plaque also hardens and narrows the coronary arteries.
CABG is one treatment for CHD. During CABG, a healthy artery or vein from the body is connected, or grafted, to the blocked coronary artery. The grafted artery or vein bypasses (that is, goes around) the blocked portion of the coronary artery. This creates a new path for oxygen-rich blood to flow to the heart muscle.
Surgeons can bypass multiple coronary arteries during one surgery.
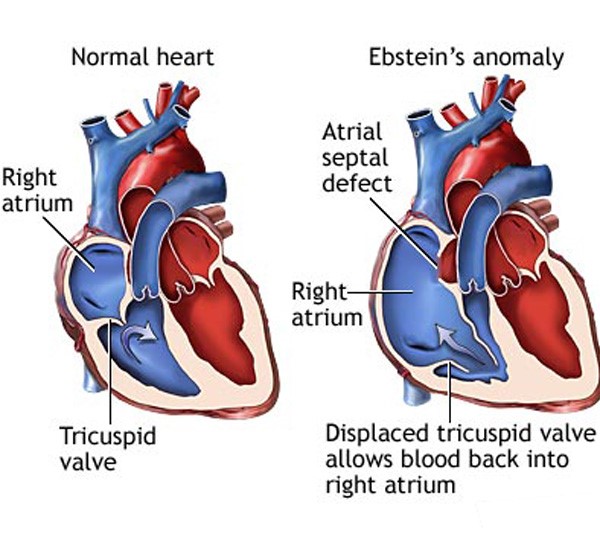
Ebstein's Anomaly
Minimal Invasive Valvular Heart Surgery with Valve Repair
Our heart is a pump and needs healthy valves to function optimally. There are 4 valves in our heart, two located between the chambers (Mitral and Tricuspid) and the other two located between the chambers and blood vessels (Aortic and Pulmonary Valves). When open, the valves allow the blood to flow only in one direction; when closed, these valves form a strong seal between the different chambers of heart as well as blood vessels.
Types of Heart valve malfunction
- Leaky Valve (Regurgiation) that enables the blood to flow in a reverse direction
- Narrowed valve (Stenosis), in which there is a narrowing, thickening and fusion of valve leaflets that restricts the blood flow across the valve.
When is Valve repair or replacement required?
It is required if the valve has been damaged due to:
- Congenital Heart Defect
- Endocarditis
- Rheumatic heart disease
- Aging/Degenerative
- Types of Valve Surgeries?
Depending upon the extent and location of damage, valves can be either repaired or replaced by different procedures like: - For Valve Narrowing (Stenosis) : Closed or open valvulotomy is performed. In this procedure, an incision is made in a fused/narrow valve to restore the valve opening. However, if the restructure of the valve is deranged then a valve replacement is done using a mechanical/metallic (St. Jude or Medtronic Valve) or a bioprosthetic (porcine valve).
- Valve Regurgitation : Advanced repair techniques are used for valve leaflets as well as subvalvular apparatus. In case, its repairing is not feasible then valve replacement is done. We are equipped with cardiac surgeons who specialize in repair techniques for regurgitant mitral valves. Valve replacement is only done for extreme structural abnormality of mitral valve.
Pacemaker Implantation
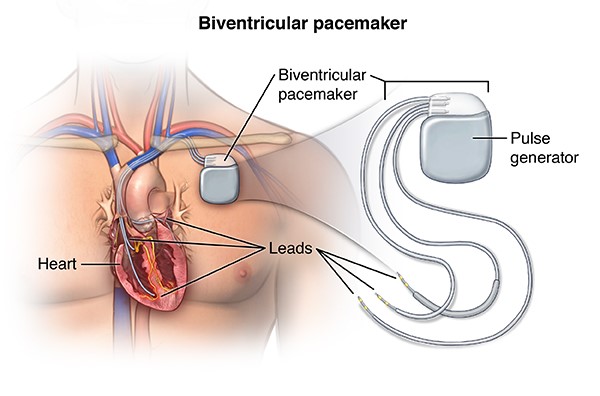
The pulse generator emits electrical impulses through the wires to your heart. The rate at which the electrical impulses are sent out is called the pacing rate.
Almost all modern pacemakers work on demand. This means they can be programmed to adjust the discharge rate in response to your body’s needs.
Implantable cardioverter defibrillators (ICDs)
If the pacemaker senses that your heart has missed a beat or is beating too slowly, it sends signals at a steady rate. If it senses that your heart is beating normally by itself, it doesn’t send out any signals. Most pacemakers have a special sensor that recognises body movement or your breathing rate. This allows them to speed up the discharge rate when you’re active. Doctors describe this as rate responsive.
An implantable cardioverter defibrillator (ICD) is a device similar to a pacemaker. It sends a larger electrical shock to the heart that essentially “reboots” it to get it pumping again. Some devices contain both a pacemaker and an ICD.
ICDs are often used as a preventative treatment for people thought to be at risk of cardiac arrest at some point in the future. If the ICD senses the heart is beating at a potentially dangerous abnormal rate, it will deliver an electrical shock to the heart. This often helps return the heart to a normal rhythm.
A conventional ICD has a pacing lead that’s implanted along a vein (transvenously). There’s also a newer type of ICD where the pacing lead is implanted under the skin (subcutaneously).
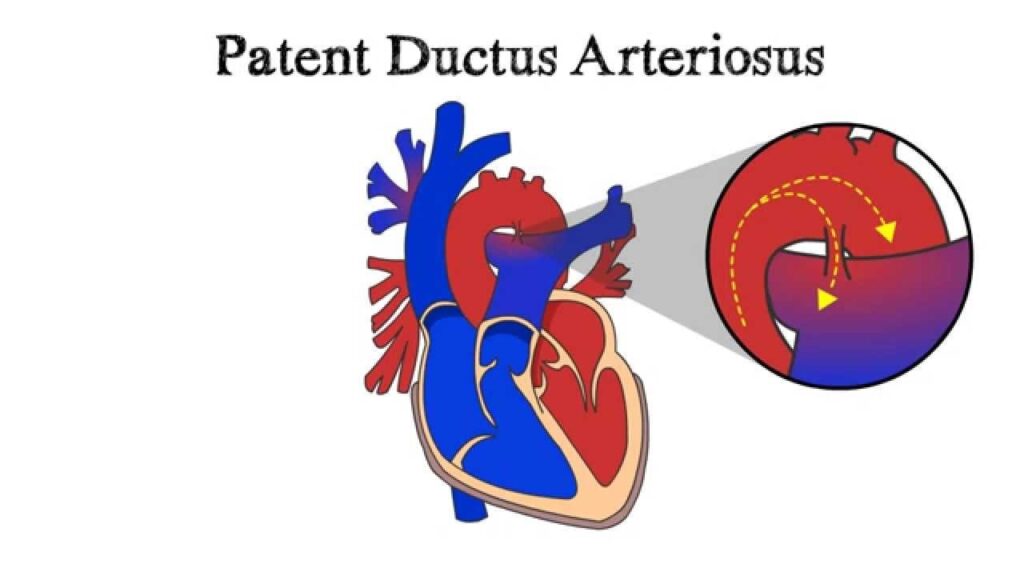
Patent Ductus Arteriosus (PDA)
Pulmonary Stenosis
Tetralogy of Fallot (TOF)

Transposition of the Great Arteries
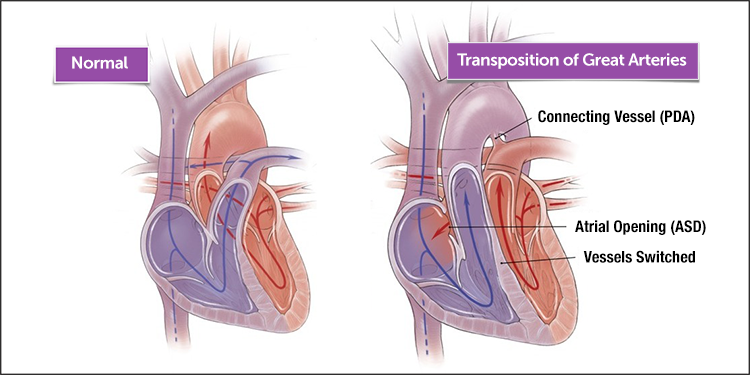
The first type is dextrotransposition of the great arteries (d-TGA), with “dextro” initially meant to describe the location of the aorta in respect to the pulmonary artery. In this condition, the right ventricle gives rise to the aorta and the left ventricle gives rise to the pulmonary artery, but both atria are appropriately connected to their respective ventricles (AV concordance). This condition is not compatible with life unless there is a naturally occurring shunt (ASD, VSD, or PDA) or surgically created shunt. Often, these patients have undergone repair during childhood with a Senning or Mustard procedure, in which blood is baffled from the venae cavae to the left atrium and from the pulmonary veins to the right atrium . The primary long-term concern in these patients is that the right ventricle is ill prepared to serve as the systemic ventricle. It can weaken and fail over time (usually when the patient enters the third or fourth decade), and these patients also develop significant systemic AV regurgitation, with the tricuspid valve in the mitral position.
The other type of TGA is the congenitally (naturally) corrected lesion, levotransposition of the great arteries (l-TGA). In this case, the ventricles are also inverted (both AV and ventriculoarterial discordance are present). This variation results in a circulation in which blood flows from vena cava to right atrium to left ventricle to pulmonary artery to pulmonary veins to left atrium to right ventricle to aorta. Again, the problem remains a right ventricle pumping into the systemic circulation. This condition is also associated with about a one in three lifetime prevalence of complete heart block.
Ventricula Septal Defect (VSD) & Closure/ Repair

A ventricular septal defect (VSD) is an opening or hole in the wall that separates the two lower chambers of the heart. This wall is called the ventricular septum. The hole causes oxygen-rich blood to leak from the left side of the heart to the right side. This causes extra work for the right side of the heart, since more blood than necessary is flowing through the right ventricle to the lungs. The hole is usually closed with surgery. However, in certain situations, your child’s cardiologist and surgeon may think it is best to close the hole with a special device. This procedure is done in the heart catheterization lab.
The procedure is performed while your child is under a general anaesthetic. This means that your child will be asleep during the procedure. Not every VSD can be closed with heart catheterization. Therefore, we first need to measure the VSD to make sure it can be closed with a device in the catheterization lab. When your child is asleep, we will do a test called a transesophageal echocardiogram. “Echocardiogram” means a heart ultrasound. “Transesophageal” means we do the ultrasound with a small probe that is placed in your child’s esophagus, the tube that connects the mouth to the stomach. This test will measure the size of the hole and help place the closure device.
If the test shows that the hole is too big to close with the device, we will wake up your child and send him or her to the recovery room. Your child’s cardiologist will discuss the next steps with you and your child.
If the hole is small enough and in the right position, we will go on with the catheterization.
During the catheterization, the doctor puts a catheter with a small deflated balloon on the tip through the blood vessel to the hole. The balloon is inflated to measure the size of the hole again. If the hole can be closed with the device, the doctor puts the closure device inside the catheter and places the device into the hole. Once the device is in place, the doctor takes out the catheter and covers the cut on your child’s leg with a bandage.

Aarav Medicare team is ready to look after all your medical emergency needs. We will Take care of your health.
Saurav
Why Aarav Medicare?

Highly Qualified Specialists
Best Specialist Doctors for all the Treatment and Procedures. Get Free Online Consutations.

State Of The Art Facility
Finest Hospitals with all the modern Medical Equipment and Best Patient Care.
